Scientific Image Gallery

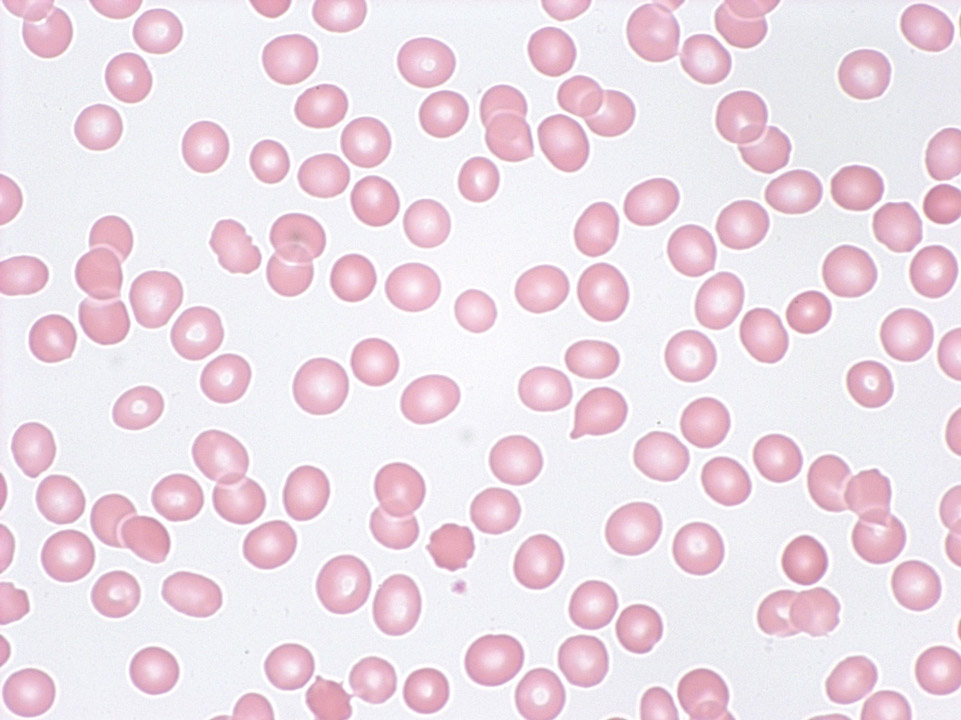
Cell description: 3 different stages of nucleated red blood cells are known: basophilic, polychromatic and orthochromatic
Size: around 10 µm
Nucleus: round with variable degree of chromatin condensation according to maturation, faint or absent nucleoli
Cytoplasm: bluish to pink (depending on maturation), no granules
Nucleus decreases in size as the cell matures
<p>Cell description: 3 different stages of nucleated red blood cells are known: basophilic, polychromatic and orthochromatic </p> <p>Size: around 10 µm </p> <p>Nucleus: round with variable degree of chromatin condensation according to maturation, faint or absent nucleoli </p> <p>Cytoplasm: bluish to pink (depending on maturation), no granules </p> <p>Nucleus decreases in size as the cell matures</p>
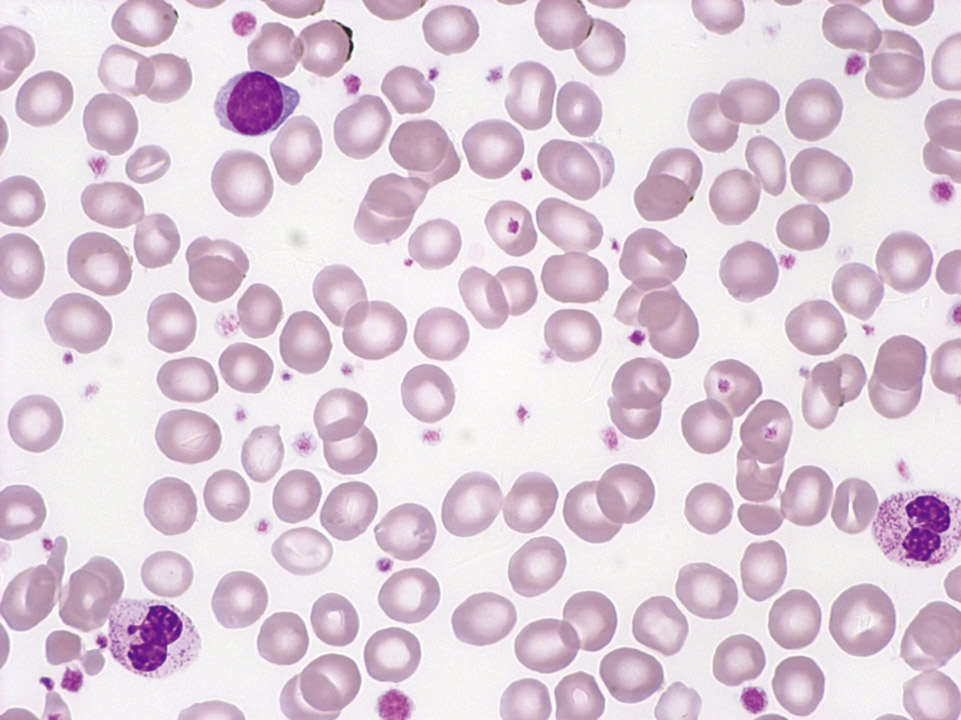
Pancytopenia (tricytopenia) in the peripheral blood (May-Grünwald-Giemsa stain) of a patient with severe aplastic anaemia: The automated cell count showed granulocytopenia (300/µL), mild lymphocytopenia (800/µL), anaemia (haemoglobin 9 g/dL), a reduced reticulocyte count (18,000/µL) and thrombocytopenia (12,000/µL).
<p>Pancytopenia (tricytopenia) in the peripheral blood (May-Grünwald-Giemsa stain) of a patient with severe aplastic anaemia: The automated cell count showed granulocytopenia (300/µL), mild lymphocytopenia (800/µL), anaemia (haemoglobin 9 g/dL), a reduced reticulocyte count (18,000/µL) and thrombocytopenia (12,000/µL).</p>
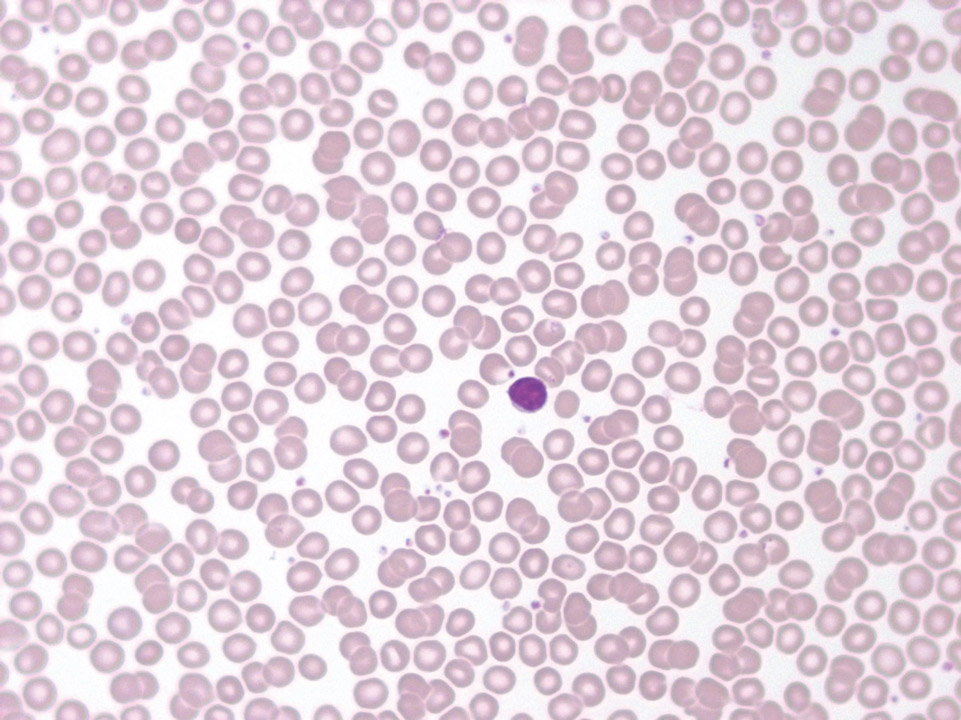
The peripheral blood (May-Grünwald-Giemsa stain) of this patient shows only isolated neutropenia (900/μL) with morphologically normal red blood cells and normal red blood cell and platelet counts. Aplastic anaemia is not present. A lymphocyte can be seen in the middle.
<p>The peripheral blood (May-Grünwald-Giemsa stain) of this patient shows only isolated neutropenia (900/μL) with morphologically normal red blood cells and normal red blood cell and platelet counts. Aplastic anaemia is not present. A lymphocyte can be seen in the middle.</p>
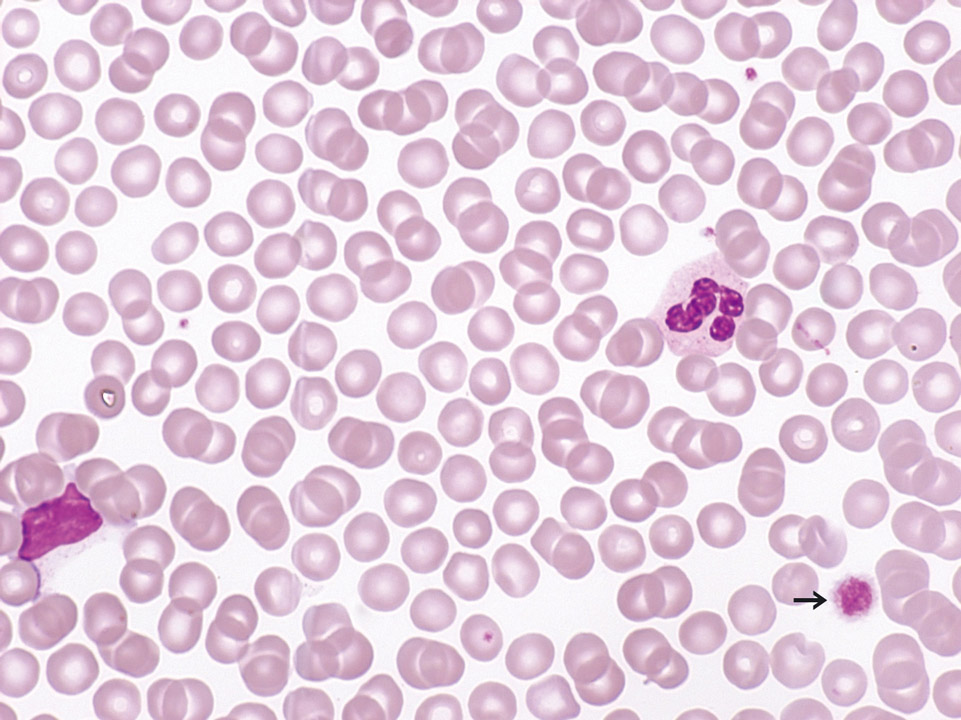
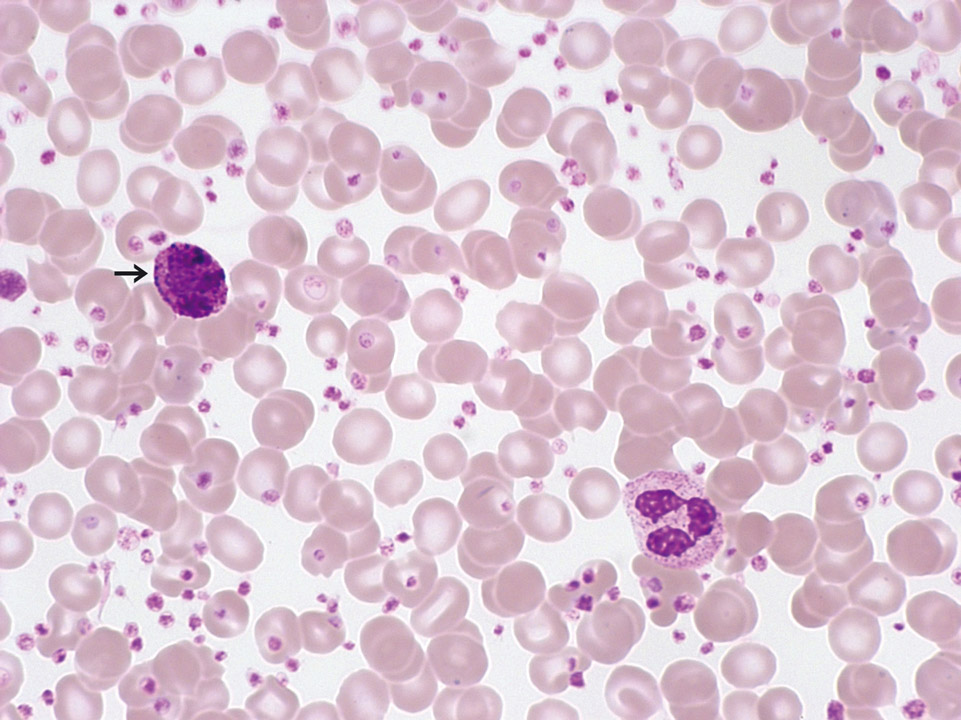
Peripheral blood (May-Grünwald-Giemsa stain) of a patient with B-CLL. The few platelets are mostly large (->) (= platelet anisocytosis). Here a secondary immune thrombocytopenia (ITP) was evoked by immunoglobulin-producing lymphoma cells. The immunoglobulins react with proteins on the platelet surface, leading to an elimination of these platelets from the peripheral blood.
<p>Peripheral blood (May-Grünwald-Giemsa stain) of a patient with B-CLL. The few platelets are mostly large (->) (= platelet anisocytosis). Here a secondary immune thrombocytopenia (ITP) was evoked by immunoglobulin-producing lymphoma cells. The immunoglobulins react with proteins on the platelet surface, leading to an elimination of these platelets from the peripheral blood.</p>
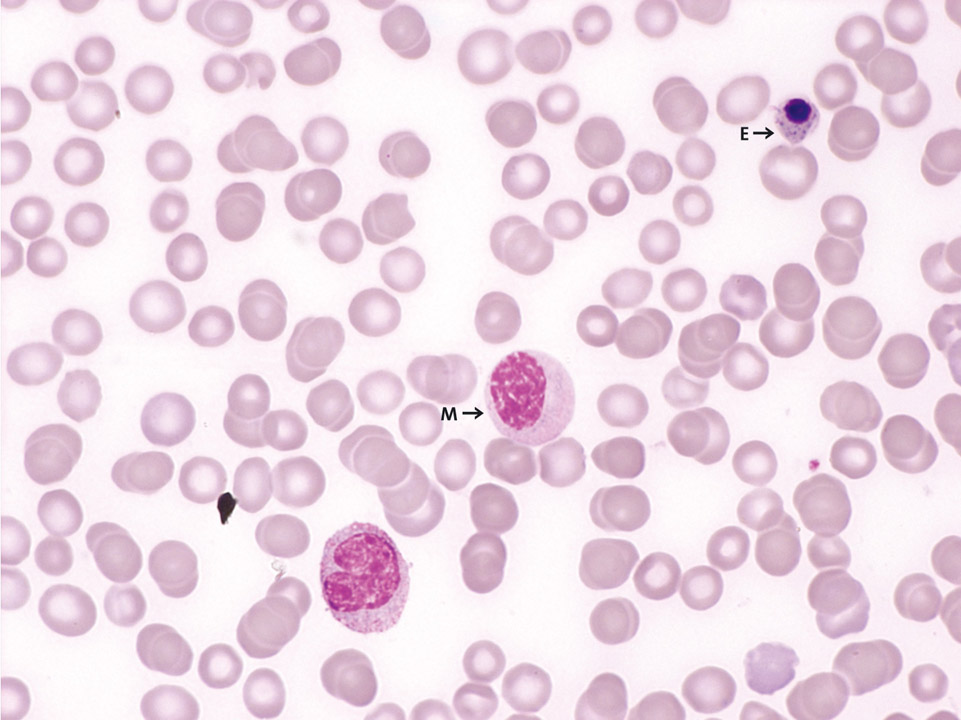
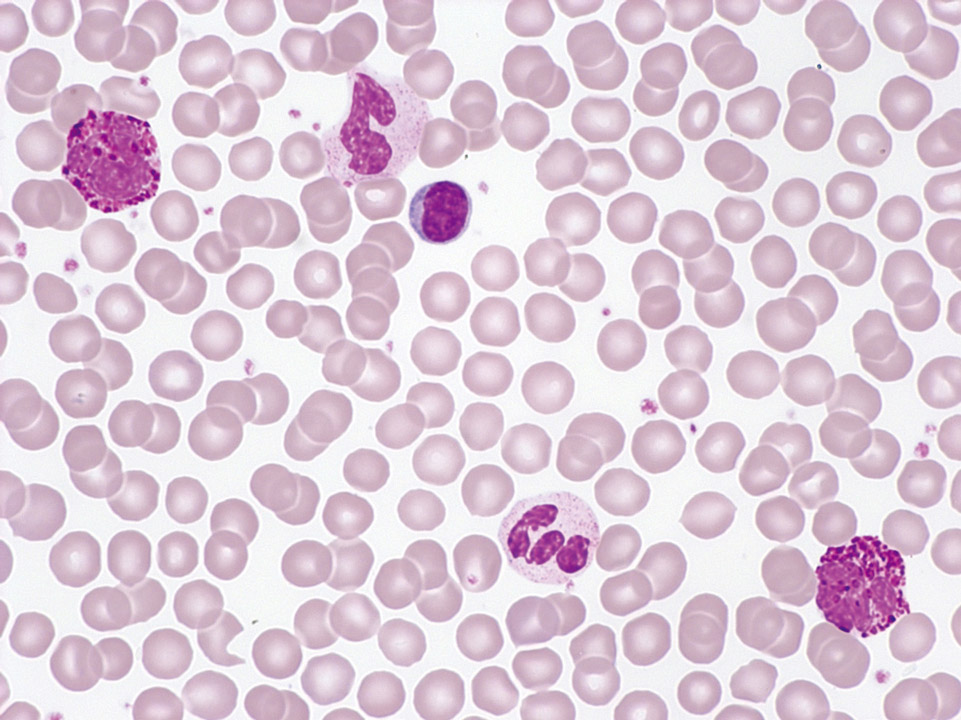
The peripheral blood (May-Grünwald-Giemsa stain) of a patient with breast cancer and bone metastases demonstrates a leucoerythroblastic picture. There are left-shifted granulopoiesis (e.g. here a myelocyte (M)), erythroblasts (E) and distinct thrombocytopenia.
<p>The peripheral blood (May-Grünwald-Giemsa stain) of a patient with breast cancer and bone metastases demonstrates a leucoerythroblastic picture. There are left-shifted granulopoiesis (e.g. here a myelocyte (M)), erythroblasts (E) and distinct thrombocytopenia.</p>
Peripheral blood (May-Grünwald-Giemsa stain) of a 27-year old patient with chronic myelogenous leukaemia (CML). Normal red blood cells, marked thrombocytosis (2,750,000/µL), increased basophilic granulocytes (->) and a normal white blood cell count are observed. In this case no JAK2 mutation could be detected; instead the patient was tested positive for the BCR-ABL fusion gene.
<p>Peripheral blood (May-Grünwald-Giemsa stain) of a 27-year old patient with chronic myelogenous leukaemia (CML). Normal red blood cells, marked thrombocytosis (2,750,000/µL), increased basophilic granulocytes (->) and a normal white blood cell count are observed. In this case no JAK2 mutation could be detected; instead the patient was tested positive for the BCR-ABL fusion gene.</p>
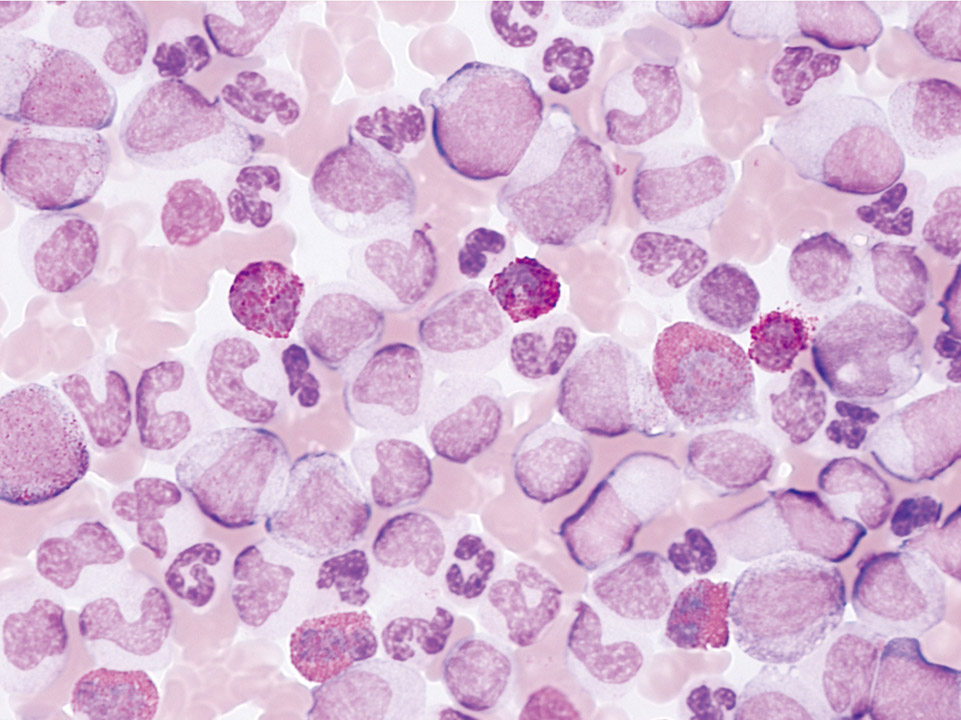
The peripheral blood (May-Grünwald-Giemsa stain) of a 27-year old patient with hearing loss showed a massive leukocytosis (680,000/µL) and a marked left shift with a distinct fraction of blast cells. Several eosinophilic cells are clearly visible. Platelets are abundant, although not visible in this part of the blood film. The BCR-ABL fusion gene was detected by FISH analysis of the peripheral blood and secured the diagnosis of CML. Because of the threat of permanent loss of hearing chemotherapy was started within hours after venepuncture (without waiting for the results from bone marrow cytology).
<p>The peripheral blood (May-Grünwald-Giemsa stain) of a 27-year old patient with hearing loss showed a massive leukocytosis (680,000/µL) and a marked left shift with a distinct fraction of blast cells. Several eosinophilic cells are clearly visible. Platelets are abundant, although not visible in this part of the blood film. The BCR-ABL fusion gene was detected by FISH analysis of the peripheral blood and secured the diagnosis of CML. Because of the threat of permanent loss of hearing chemotherapy was started within hours after venepuncture (without waiting for the results from bone marrow cytology).</p>
The peripheral blood (May-Grünwald-Giemsa stain) of a patient shows as an incidental finding leukocytosis with left shift up to myelocytes, basophilia and mild thrombocytosis. CML was suspected and later confirmed by cytogenetic demonstration of the Ph1.
<p>The peripheral blood (May-Grünwald-Giemsa stain) of a patient shows as an incidental finding leukocytosis with left shift up to myelocytes, basophilia and mild thrombocytosis. CML was suspected and later confirmed by cytogenetic demonstration of the Ph1.</p>
Peripheral blood (May-Grünwald-Giemsa stain) of a patient with ET showing an isolated thrombocytosis. A JAK2 mutation was detected by molecular biological techniques. The BCR-ABL fusion gene was not found.
<p>Peripheral blood (May-Grünwald-Giemsa stain) of a patient with ET showing an isolated thrombocytosis. A JAK2 mutation was detected by molecular biological techniques. The BCR-ABL fusion gene was not found.</p>